Let’s talk October 2019 and PDPM. I've been sitting on this one for a while...
In fact, I was debating about whether I should talk about it at all. I asked myself "Will practitioners even read this? They won't think I understand." I also kept approaching my finger toward the "record" button on my phone to do this on live broadcast via Facebook ...then after hesitating on that, I thought about writing it in a instagram post...I definitely said to myself "maybe I should just let this play out on its own accord and not have anything to do with the influence and direction of where the future of our profession goes."
As I was debating all of this, I found that I cannot just sit on it anymore. It's days away from being here and I promised myself I would honor and care for my occupational therapy colleagues when they are faced with a roadblock.
I risk being shamed for this by some practitioners because they are not ready; ready to take on more work... and frankly too exhausted to fight the good fight. I get that; it’s been a lot... but my desire to get these tips out to you are worth it because I promised to mentor and look out for practitioners like you that need guidance in an uneasy time (especially when facing barriers like the uncertain ones to come at this time in the profession).
We are talking about shifts in payment for treating clients; within skilled nursing facilities (come October) and soon after in home health settings (January).
This post is for you if you want to know what you can do about the changes.
This article is not for you if you expect things to change on their own or do not have the energy to do the work ahead of you.
I want to first start out by identifying one common theme that is happening amongst us:
fear of the UNKNOWN
There are a lot of questions spiraling around including:
** My boss is not telling us much; we don't really know what to expect. What do I do?
** Will I have a job after this?
** I was already laid off before it began. Now what? Do I just look outside of the profession to pay the bills? I have a family and myself to feed.There are no jobs in a 40 mile radius.
** They’re expecting me to do more work with less. How is this even possible?
** Will I have a job after this?
** I was already laid off before it began. Now what? Do I just look outside of the profession to pay the bills? I have a family and myself to feed.There are no jobs in a 40 mile radius.
** They’re expecting me to do more work with less. How is this even possible?
** I've been down this road before, it's all the same.
** Group treatments? There’s only so many allowed in the new payment structure!
** (insert dilemma and disappointment here).
** what about the ethical issues? They'll just look different now.
** Group treatments? There’s only so many allowed in the new payment structure!
** (insert dilemma and disappointment here).
** what about the ethical issues? They'll just look different now.
Feeling scared, tired, sad, mad, upset and lost is reality of change. When there is change brewing in payment sources, our first gut reaction is to wonder what's next for our careers, financial future and mental well-being as practitioners.
There is no doubt that this transition, like any in life, is EXTREMELY DIFFICULT for those who work in those settings. In fact, it is not just those settings...I personally fear (as I go about my day working in acute care) that not all my clients will have opportunity to be accepted at skilled nursing facilities once the dust settles. It is this weird fear of mine that creeps up that less clients will be accepted to SNF and home health if we do not understanding how to get them accepted under the new payment structure. I fear that it will be just as hard to get clients into SNF settings as it is to get them into acute rehab...I thought, "oh no! what if my client doesn't have a discharge plan after their care?"...fears
...fears from the unknown.
There is uncertainty about the future from all angles due to this transition coming.
But that is exactly what it is, a transition...a different direction...and here's some real talk:
every TRANSITION in life is difficult
It is difficult because it is uncomfortable. I've mentioned this in a podcast episode I spoke on (with the transparent Brock Cook from the Occupied Podcast), that there is discomfort because we are stretching and growing into something different than we are already familiar with. On a physiological level, we like to know we are safe and that this, like anything else, won't hurt.
I guarantee you, you are not the only one feeling it: aside from physical therapists and speech-language pathologists, your facility staff, including nursing and physicians, as well as your boss and non-therapy administration, will also be going through some growing pains as they process what is coming.
That is why I want to challenge you to step out of your comfort zone. Step out a wee bit farther than being forced to by external factors right now. This is to shift that "scary" change into a transformation you can look forward to.
Let me emphasize a point here:
with change ALSO comes transformation
So, what is Transformation?:
Transformation is an opportunity to shift into something better, especially from the beginning stages.
Think about going from a caterpillar to a butterfly. The butterfly must struggle to get out of the cocoon. They must do so on their own or it risks its life and dies when forced from its shell.
You must struggle to get the wiggle room you desire to fly in your career.
The freedom to fly stems from YOU; when you decide to move in the direction of opportunity (which takes somewhat of a struggle to get to). It means the struggle we choose to endure (with the goal of achieving the desired direction we want to go) allows you the freedom to fly anywhere you want.
So what does that struggle look like in order for you to fly?:
First, it's not getting up and leaving the profession right away.
Therapy Practitioners: Whatever you do, if you have not been let go, actually even if you have been let go, DON'T FLEE.
Travel therapists: If you cannot find a travel assignment because facilities are halting their contracts, DON'T FLEE.
If you do, you have already decided to reject the future of the profession and reject any opportunity that may exist. Instead of fleeing, try walking into it more deeply.
- Step into these meeting rooms where the conversations are being had.
- Build a seat at the table to discuss how your facility will be handling the changes.
- Be involved in the conversations (without asking for permission).
- Ask the hard questions.
- Initiate the narrative around what you have found out so far about PDPM and how you can help.
This is your opportunity to share your ideas about how to help with the transition; from an OT lens and right from the beginning.
Have a judge-free dialogue about the current state of the facility or it's operators. Talk freely about what these changes mean for who, while discussing how to utilize each resource in the interdisciplinary staff to get the goals for reimbursement accomplished. After all, the interdisciplinary approach will be more crucial than ever.
Your first struggle in this though is:
You'll be out of your comfort zone
Might as well step out of your comfort zone on your own time rather than the decision being made for you by being let go (before making your voice heard). Make the decisions alongside your boss or admin (as they are finding out that they do not know all the answers either). The unknown is sort of a blessing because it means there is also a blank canvas to create on; take advantage of painting on it. The facility decision makers are also needing to step out of their comfort zones just the same. Taking a leap, have an impact on that leap and jump together to create a masterpiece.
You next struggle is:
Acting like a boss
Instead of waiting for your boss to tell you what comes next with these changes, be the change. This change come October will allow you permission to be a partner alongside them to address the changes. Respectfully act like an owner, showing you are invested in the health of the company. Instead of submitting to an employee role below the hierarchy, be a partner.
Your third struggle:
Going back to your roots
You'll be a little rusty and that is okay. However, after you dust yourself off, forgive yourself for doing all that "THER EX" and gather your resources to learn the ropes of what is to come; you will be able to provide your perspective of what OT does for patient driven care. With a bit of trial and error, you will discover along the way what has to happen in order to create and establish an interdisciplinary approach, together.
I know it’s not easy (I’ve been there with my own hurdles in practice, achieving a voice for OT, and making forward movement); but
It is truly, truly simple and it is glorious when you get to enjoy the fruits of your labor (because you did the work).
For many of our peers (and maybe you feel this as you are reading this now) you feel it’s the end of your career because you are tired, you've been through this rodeo already, and this is hard. For some of you, you will tell me "but they.......(insert past burn they placed upon you here)" This is different because you are all starting from scratch. It is the very beginning of everything you had hoped for in your profession when you started.
If you wait for your boss to tell you what to do, you are waiting on someone else’s opinion of the subject matter. Truth is, this is new to them too and THEY NEED YOUR help and expertise about what patient's want in order to achieve their outcomes. Show them what they do not know yet. They need you to show up at the table where decisions are being made and for you to collaborate with them...before they come to the conclusion that what you offer doesn't serve the company (because they cannot see it) you have to show them.
So how do you do this? How do you show your worth to your boss and administrators?:
1. Go back to your roots.
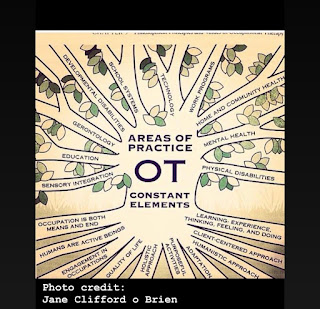
Utilize your skill set to help your facility through the transition: whether that is using the OTPF or pulling from the Occupational Profile to get back in touch with the framework of what we do, reference what we know and how that speaks to the patient driven outcomes. In fact, our OT evaluation complexity codes require us to address the occupational profile in order to be reimbursed anyways. This portion should not be so bad to get used to.
Also, consider joining the hub of treatment ideas and support for working with older adults over at Seniors Flourish Learning Lab (as an affiliate, you enjoy 10% off the subscription with use of this link or use of the code " ALEXISOT:111 " at checkout)
2. Seek information from the source, not peers.
Now if you are not into technical things, flipping through the many pages of CMS may not be an ideal way to do some more research. That's what is so incredible of our own national association's efforts during this transition time. They have support conversations over at communOT, an entire page dedicated to seminars and CEU opportunities about how to equip yourself during this time, grasping an understanding for PDPM and what it means in terms of your role as a practitioner.
...and as a member of the association, you also have many other resources at your fingertips to stay prepared. My sharing of AOTA's resources is not sponsored and I do not work directly on any committee or board of theirs; I am solely an everyday member, like some of our own colleagues are. I have simply seen the hard work they have pursued to give you the tools to get the work done with during this time. In fact, a fellow OT I have known for many years (through my own state association, as well as admiring their representative involvement in staying in the know of governmental affairs), is actually one of the presenters in one of the seminar trainings to get practitioners ready for PDPM.
Allow the associations to help you. Join them, look at what they are offering you and invest in the tools they have worked hard to develop FOR you.
Learn EXACTLY what you need to know to navigate these new waters over at their main PDPM page
3. Invest in a mentor.
This is critical; we need an outside party we trust to support us when we feel lost and when we need some additional tools to navigate. If you do not have a mentor, stick it out with me into 2020 because I have something coming up for you. My mentor program will be relaunching to help walk alongside you during the uneven terrain you're about to travel.
It will be there for you to help guide you during those hard transitions throughout the ups and downs.
To stay informed of when the mentor program will be re-released, and to receive notice of my current free trainings, updates on what's happening in the world of OT and more, get yourself on my email list to stay informed. Go to creatingconfidentots.club
If I'm not your mentor or you need on the ground, face-to-face support, I'm not offended. I care less about who you go to and more about whether that person is:
- external from the context of your work
- are real with you when they need to call you out (or to admit when they don't know something)
- admit their mistakes when they have made them
- have your back in tough times
- are there to elevate your practice as you grow
Closing thoughts...
This change in healthcare will likely not be the last change; life is fluid... it keeps moving and changing. We need someone by our side during those ebbs and flows.
We need this change inside of us to get to the next level of how we show up and care for our clients.
Now is the time to make one of two decisions:
Invest in being informed of how to navigate this; move one foot in front of the other, alongside each other, as one profession
or
walk out the door onto your new journey
The choice is always yours.
with love, Lex